Glaucoma Diagnosis & Testing
Diagnosing Glaucoma can be achieved by examining the optic nerve and it’s capability to efficiently relay visual information to your brain. A full workup can determine damage to the optic nerve and can advise the physician of the severity of the disease. With specialized instruments and techniques, this can aid the physician in properly diagnosing the condition of your eye and assisting in your care.

Measuring your Eye Pressure
Elevated optical pressure is a good indicator of likelihood of having glaucoma. In this exam, we will utilize various instruments to measure your eye pressure such as a Tonometer.
I-care Tonometer
The I-care Tonometer is a light-weight probe that facilitates the ability to check your eye pressure without requiring air or eye drops. This newly customized technology makes momentary contact with the cornea, which per patient’s feedback, is rarely felt, and confirms your intraocular pressure.
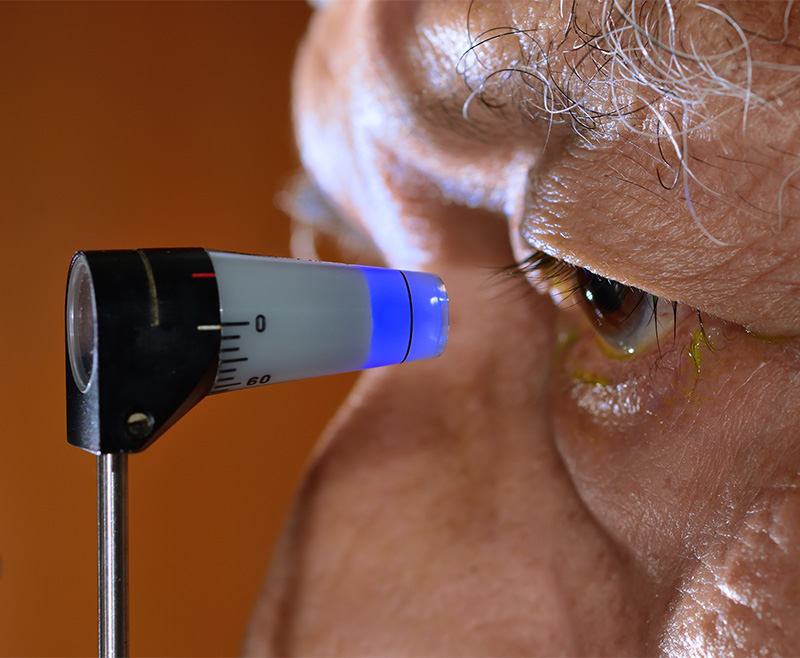
Applanation Tonometer
Applanation Tonometer is a device used to apply a certain amount of force to momentarily flatten part of the cornea. This exam checks the patient’s intraocular pressure and allows the physician to determine glaucoma development.
Diagnostic tools
Pachymetry
The physician utilizes a device called a pachymeter that is used to check the thickness of your corneas. This is an important factor in determining whether or not you have glaucoma as it will allow the doctor to more accurately determine your eye pressure. If you have thicker corneas then you are more likely to have lower and safer eye pressures. Alternatively, if you have thin corneal thickness it may represent higher pressures. It is important to get evaluated because it can lead to misdiagnosis of glaucoma.
Gonioscopy
Visual Field Exam:
The most common visual field exam is the Humphrey visual field machine. This is a reliable way to determine your eyes ability to see flashing lights out of your peripheral vision. This exam is a vital source for a physician to evaluate the progress of your vision to monitor any developing glaucoma. The visual field exam creates a summary of the number of flashing lights noted and incorporates it into a optical image of what you see, any gray or darkened areas represent missing counts of flashing lights that may be due to glaucoma damage.
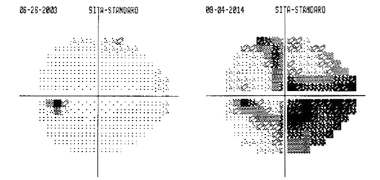
The image on the left notes a healthy normal visual field. The black spot is the “blind spot” that is found on both eyes.
Fundus Photography
Fundus Photography is a way to evaluate the inside of the eye and monitor the optic nerve. It is an excellent source of evaluating for possible signs of improving or worsening glaucoma called glaucomatous cupping. The cupping is referred to when nerve cells near the optic nerve begin to surround the “hole” instead of covering it like a thin piece of tissue. This represents loss of healthy nerve tissue that make up your peripheral vision. Loss of peripheral vision is not apparent until severe damage has been done.
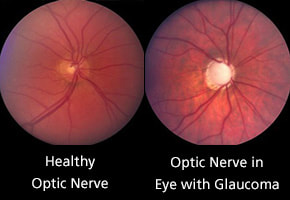
These photographs are able to capture this occurrence, and would usually be taken annually or as needed by your opthamologist to compare future examinations with previously taken photographs.
Dr. Velasquez prefers a conservative approach to treating glaucoma and performs surgery only when indicated. He has a special interest in minimally invasive glaucoma surgery performed at the time of cataract surgery.

Request an Appointment
Main Clinic- Castle Hills
6810 West Avenue, Suite A
San Antonio, Texas, 78213
Surgery Center- American Surgery Center
12838 Vista del Norte
San Antonio, TX, 78216
Monday – Friday
Phone
Fax